Breast density and you!
Dense breasts and breast cancer screening — what does it mean for you?
If you’ve recently had a mammogram and been told you have dense breasts, you’re not alone — and you’re certainly not doing anything wrong. Dense breasts are very common, completely normal, and something many women only learn about once they start mammogram breast cancer screening.
But what does it actually mean? And does it change how you should approach breast cancer screening? Let’s break it down.
What does it mean to have dense breasts?
Breasts are made up of two main types of tissue:
Fibroglandular tissue (the milk ducts and supportive tissue)
Fatty tissue
When a mammogram shows that a person has more fibroglandular tissue than fatty tissue, their breasts are described as dense.
You can’t feel breast density, and it has nothing to do with breast size, firmness, or how your breasts look. Density is only visible on a mammogram.
Routine mammographic screening through BreastScreen Australia is recommended for asymptomatic women aged 50-74 years and is available for women 40-49 years and over 74 years if they choose to screen. This cancer screening program is fully subsided by Medicare so there are no out of pocket costs.
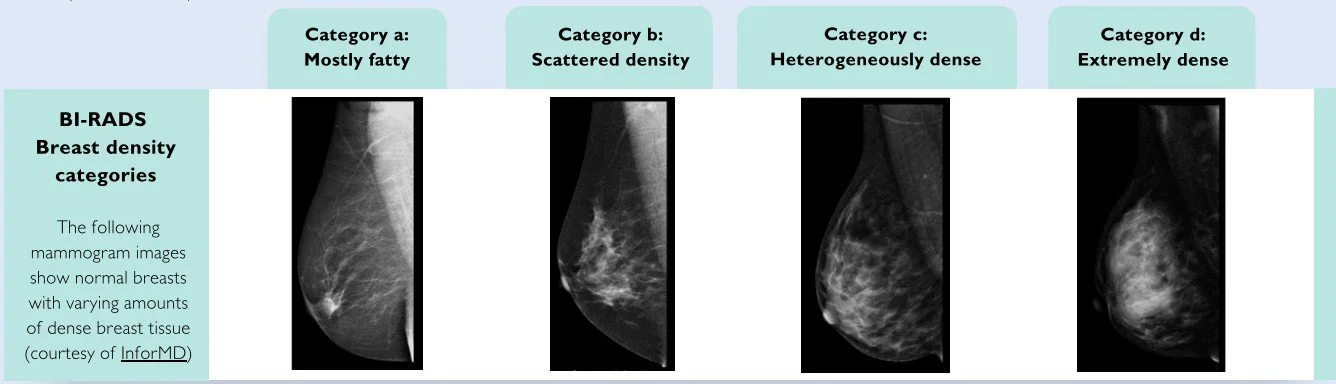
Breast Density is reported as A,B,C or D.
Why does breast density matter?
There are two key reasons breast density is important.
1. Dense tissue can make mammograms harder to read
On a mammogram:
Dense tissue appears white
Breast cancers also appear white
So dense tissue can mask cancers, making them harder to detect. Mammograms still reduce breast cancer deaths, but they are not quite as sensitive in dense breasts.
The sensitivity of screening mammography (that is, the percentage of women with cancer who attend screening and are correctly identified as having cancer) is approximately 90% for women with low breast density (classified as BI-RADS a or b), 84% for women with dense breasts (BI-RADS c) and 64% for women with extremely dense breasts (BI-RADS d)
2. Dense breasts slightly increase breast cancer risk
Women with extremely dense breasts have a higher‑than‑average risk of breast cancer. It’s not a dramatic jump, but it’s enough that it should be considered alongside your other risk factors when planning your breast cancer screening.
As a group, women with BI-RADS category a have around half the risk for breast cancer than women with BI-RADS category b, while those with BI-RADS category c and d have 1.6-fold and 2.6-fold higher risk, respectively, than women with BI-RADS category b.
How common is increased breast density?
Very common.
Around 40–50% of women have dense breasts. (Category c aprox 40%, Cat d aprox 10% of the screening population) It’s especially common in:
Younger women
Women who are perimenopausal
Women using menopausal hormone therapy
Breast density often decreases with age and post menopause, but not always.
Does having dense breasts mean I need extra screening?
Not automatically. Breast density is one part of your overall risk picture. Other factors matter too, such as:
Age
Being overweight
Family history of breast or ovarian cancer
Known genetic variants (e.g. BRCA1/2)
Previous breast biopsies or high‑risk lesions
Lifestyle factors - including exercise (reduces risk), drinking alcohol (increases risk)
For those at average risk of breast cancer, regular 1 or 2 yearly 2D mammography remains the recommended screening tool.
For those at moderate or higher risk and/or category d breast density, additional imaging may be considered. This is where a personalised discussion with your GP becomes important.
Understanding your personal risk: the iPrevent tool
If you’d like to understand your individual breast cancer risk more clearly, there is an Australian online tool called iPrevent.
What is iPrevent? iPrevent is an evidence‑based breast cancer risk assessment tool developed in Australia. It can estimate your personal risk of developing breast cancer and suggest risk‑management options.
You can access it online “iPrevent breast cancer risk assessment tool”. Many women find it helpful to:
Complete iPrevent at home
Print or save the summary
Bring it to their GP appointment to guide a more tailored discussion
Your GP can then interpret the results with you and help decide whether you sit in an average, moderate, or high‑risk category — and what that means for your screening plan.
Additional screening options: what they are, and their pros and cons
If you have dense breasts, you may hear about other imaging options beyond standard mammography. Here’s a practical overview.
Mammography 3D/tomosynthesis (Digital Breast Tomosynthesis, DBT)
What it is: Low‑dose X‑ray of the breasts. 3D mammography (tomosynthesis) takes multiple images in thin slices, which can improve cancer detection in dense breasts.
Pros:
Proven to reduce breast cancer deaths
Widely available, though not all BreastScreen clinics provide this, many in NSW only have 2D mammogram.
Good at detecting calcifications (a common early sign of cancer)
3D mammography can improve detection and reduce call‑backs in dense breasts
Cons:
Less sensitive in dense breasts (cancers can be hidden by dense tissue)
Uses a small amount of radiation
Can be uncomfortable due to breast compression
May incur costs if referred to a private radiology provider
Breast ultrasound
What it is: Uses sound waves to create images of the breast tissue. Often used as a supplement to mammography, not a replacement.
Pros:
No radiation
Can see some cancers that may be less obvious on mammogram, especially in dense tissue
Useful for investigating a specific lump or area of concern
Cons:
Higher rate of false positives (finding things that look suspicious but are benign)
Can lead to more biopsies and anxiety
Operator‑dependent (quality can vary)
Not routinely recommended as a screening test, more useful when there are additional risk factors or specific areas of concern.
Breast MRI
What it is: Uses strong magnets and radio waves to create very detailed images of the breast. Often done with contrast dye injected into a vein.
Pros:
Very sensitive — excellent at detecting cancers, especially in high‑risk women
Not affected by breast density in the same way as mammography
Funded by Medicare for some people considered at significantly increased risk (for example, certain gene carriers)
Cons:
More expensive and less widely available
Can lead to more false positives and biopsies
Requires an injection of contrast
Not usually recommended for average‑risk women with dense breasts alone
MRI is recommended for women with moderate to high overall risk and dense breasts. However, Medicare only funds MRI for those with a lifetime risk estimation of breast cancer of >30% (or a 10-year absolute risk estimation >5%). Paying for a breast MRI privately costs around $700-1000.
Contrast‑enhanced mammography (CEM)
What it is: Contrast‑enhanced mammography combines standard mammography with an intravenous contrast agent (a dye injected into a vein). The contrast highlights areas of increased blood flow, which can occur when cancers grow and develop new blood vessels.
You still have a mammogram, but the images are processed to show both the usual breast structure and areas where the contrast has accumulated.
Pros:
More sensitive than standard mammography alone in dense breasts
Can help detect cancers that may be less visible on regular mammograms, particularly in dense breasts
Often more accessible than MRI in some areas
Uses familiar mammography equipment, which many women are already used to
Cons:
Requires an injection of contrast, which carries a small risk of allergic reaction or kidney‑related issues in susceptible people
Involves more radiation than a standard mammogram (still within accepted medical limits)
Not yet available everywhere and not routinely used as a population screening tool
Like other sensitive tests, it can pick up findings that turn out to be benign, leading to extra tests or biopsies
CEM is an evolving tool and may be considered in specific situations as an alternative to breast MRI. There is currently no Medicare rebate for CEM testing and paying for it privately costs around $450-600.
So which additional test is “best”?
There is no single “best” test for everyone with dense breasts.
The right approach depends on:
Your overall breast cancer risk (not just density)
Your age and health and family history
Your previous imaging results
Your personal preferences around benefits vs. potential downsides (like extra tests or anxiety)
This is a complex and evolving area, which is why a personalised discussion with your GP is so important!
What can I do if I have dense breasts?
Here’s a practical way to think about it:
Don’t panic — increased breast density is common and not a diagnosis
Keep up with regular mammograms — they still save lives, even in dense breasts
Know your breasts — if something feels new or different, get it checked, regardless of when your last mammogram was
Consider using iPrevent to understand your personal risk
Talk to your GP about whether additional imaging (ultrasound, MRI, or contrast‑enhanced mammography) is appropriate for you
The bottom line
Dense breasts are a normal variation, not a reason to feel alarmed. But they do mean it’s worth having a thoughtful, personalised conversation about your breast cancer screening plan.
If you’ve been told you have dense breasts and you’re unsure what to do next, we’re happy to sit down with you, look at your mammogram report, go through your risk factors (including iPrevent results if you’ve used it), and discuss whether any additional screening options are worth considering.
You are unique — your breast cancer screening plan should be too.